If you shoot for the stars, sometimes you might actually reach them.
Just ask a multidisciplinary team of Johns Hopkins researchers who recently created a new computer program that can strongly predict a patient’s response to a particular immunotherapy drug for melanoma. The program, dubbed AstroPath, is based on a previously developed algorithm that analyzed millions of telescope images to create a precise digital map of the universe.
Sloan Digital Sky Survey
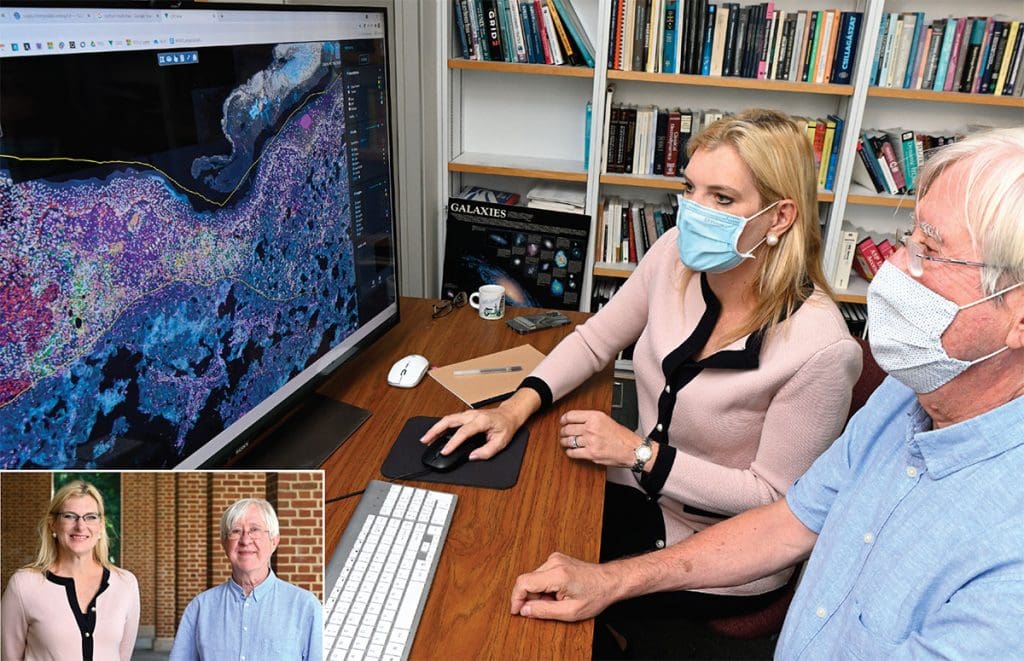
Launched back in 2000, the Sloan Digital Sky Survey was designed by Bloomberg Distinguished Professor and astrophysicist Alexander Szalay. The sky survey “stitched” together millions of telescopic images of billions of celestial objects. Each object expressing distinct signatures. Just as the Sloan Survey maps the cosmos on an astronomical scale, Hopkins Medicine researchers worked with Szalay to map tumor and immune cells on a microscopic scale.
“In astronomy we often ask, ‘What is the probability that galaxies are near each other?’” says Szalay, director of the Institute for Data Intensive Engineering and Science. “We apply the same approach to cancer. Looking at spatial relations in the tumor microenvironment. It’s the same problem on a vastly different scale.”
The team’s “big data” approach could potentially provide personalized, therapeutic guidance for many cancers, says Drew Pardoll, director of the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
“This platform has the potential to transform how oncologists will deliver cancer immunotherapy,” Pardoll says. “For the last 40 years, pathology analysis of cancer has examined one marker at a time, which provides limited information. Leveraging new technology, including instrumentation to image multiple markers simultaneously, the AstroPath imaging algorithms provide 1,000 times the information content from a single biopsy than is currently available through routine pathology.”
How the Platform Works
To generate images for AstroPath to analyze, tumor biopsy slices are bathed in antibodies tagged with fluorescent markers of different colors. Each indicates the presence and prevalence of a different protein in the biopsy. Together, the six protein markers create a colorful, glowing landscape. The landscape is replete with data on the quantities and spatial relationships of the various components of the tumor and its immediate environment.
“The spatial arrangements of different kinds of cells within tumors are important,” says Janis Taube. Taube is co-director of the Tumor Microenvironment Laboratory at the Bloomberg~Kimmel Institute and co-led the Johns Hopkins team with Szalay.
“Cells are giving each other go/no-go signals based on direct contacts as well as locally secreted factors. Quantifying the proximities between cells expressing specific proteins has the potential to reveal whether these geographic interactions are likely transpiring and what interactions may be responsible for inhibiting immune cells from killing the tumor,” Taube notes.
After biopsies were taken and imaged, patients were given an immunotherapy drug called anti-PD-1 therapy. Then the team tracked their outcomes. Those outcomes were then correlated with their biopsy images and analyzed by AstroPath to search for predictive patterns. The team found that a particular pattern and prevalence of the six proteins on specific cells in the tumor could strongly predict which patients would respond to and survive after anti-PD-1 therapy.
Changing Therapeutic Guidance
The researchers, whose study was published in Science, are already applying their findings to lung cancer. They are hopeful that AstroPath may eventually provide therapeutic guidance for many other cancers.
“Big data is changing science. There are applications everywhere, from astronomy to genomics to oceanography,” says Szalay. “The technical challenge we face is how to get consistent, reproducible results when you collect data at scale. AstroPath is a step toward establishing a universal standard.”




